Westend61/ Getty Images
Kalça displazisi olan bebekler veya evcil hayvanlar hakkında bir şeyler duyabilirsiniz, ancak bu yetişkinleri, özellikle genç kadınları etkileyebilir.
Kalça displazisini duyan insanlar genellikle bunu bebekler ve köpeklerle bağlantılı olarak düşünürler. 1000 bebekten biri kalça displazisi ile doğar, ancak bunların sadece yüzde 12'si 2 aylıktan sonra dengesiz kalçalara sahiptir [kaynak: Ramsey ]. Kalça displazisi köpeklerde , özellikle büyük ırklarda yaygındır . Kalça displazisi sadece bebeklerde ve evcil hayvanlarda görülmez. İnsanlar, özellikle kadınlar , yetişkin olduklarında kalça displazisi teşhisi konulabilir ve tedavi edilebilir.
Kalça displazisi, kalça soketini veya asetabulumu ve uyluk kemiğini veya femuru etkileyen anormal bir durumdur . Kalça displazisi olan bir kişide, kalça soketi çok sığdır veya femur yanlış yerdedir. Tarihsel olarak, birçok doktor kalça displazisini konjenital kalça displazisi (CDH) olarak adlandırmıştır. Bununla birlikte, son on yılda , kalçanın gelişimsel displazisi (DDH) kabul edilen terim haline geldi, çünkü kalça displazisi doğumdan itibaren var olabilir veya yaşamın ilk birkaç haftasında, ayında veya yıllarında gelişebilir [kaynak: Larson ve ark . ]. DDH'li tüm insanların yüzde sekseni kadındır [kaynak: Ramsey ].
Doktorlar, bebekleri hastaneden eve göndermeden önce kalça displazisini kontrol eder - yenidoğanlarda kolayca tedavi edilebilir bir durumdur. Ancak kalça displazisi erken yaşta tespit edilip düzeltilmezse, kalça hizasındaki uyumsuzluk nedeniyle kalça sağlığı zamanla bozulacaktır. Durumun ciddiyetine bağlı olarak bu, ağrı, osteoartrit, yürüme güçlüğü veya yürüyememe ile sonuçlanabilir. Ayrıca bir kişinin temel yaşam kalitesinde belirgin bir bozulmaya da katkıda bulunabilir.
Bir bebeğin gelişimi, yeterince derin olmayan bir kalça soketine nasıl yol açabilir ve doktorlar sorunu tedavi etmek için ne yapabilir? Birisi yetişkinken kalça displazisi olduğunu keşfederse, tedavi seçenekleri nelerdir? Bu ve diğer soruların yanıtlarını bu makalede öğreneceksiniz. Kalça anatomisine ve kalça displazisi olan bir kişide nasıl değiştiğine bir göz atarak başlayacağız.
- Kalça Displazisi ve Kalça Anatomisi
- Kalça Displazisi Belirtileri ve Önlenmesi
- Bebek Kalça Displazisi Teşhisi
- Erişkinlerde Kalça Displazisi Tanısı
- Çocuklarda Ameliyatsız Kalça Displazisi Tedavisi
- Erişkinlerde Ameliyatsız Kalça Displazisi Tedavisi
- Kalça Displazisi Ameliyatı
- Bernese Osteotomi veya Ganz Prosedürü veya Periasetabular Osteotomi (PAO)
- Femoral Osteotomi (FO)
- Kalça Displazisi İçin Kalça Protezi
- Kalça Protezi Revizyonu ve Kalça Yüzey Yenileme
Kalça Displazisi ve Kalça Anatomisi
Kalça displazisinin nasıl oluştuğunu ve doktorların bunu nasıl tedavi ettiğini anlamak için kalça ekleminin kendisi hakkında biraz bilgi sahibi olmanız gerekir . Kalça, soket içinde bilyeli bir eklem veya bir enartrozdur . Femurun yuvarlak başı, asetabulumun yuvasına uyan topu oluşturur. Kalça, alt ekstremite kemikleri ile gövde ve pelvisin eksenel iskeleti arasındaki birincil bağlantıyı oluşturur.

Tipik kalça anatomisi
Üç pelvik kemik - ilium, ischium ve pubis - asetabulumu oluşturmak için bir araya gelir. Bir kişi 25 yaşına gelene kadar eklemin kendisi tam olarak kemikleşmeyebilir veya kemiğe sertleşmeyebilir, bu da kalça displazisi tedavisinde erken teşhisin önemli olmasının bir nedenidir. Güçlü, kaygan bir artiküler hiyalin kıkırdak tabakası, eklemin her iki yüzeyini de tamamen kaplayarak daha düzgün hareket etmesine yardımcı olur. Labrum adı verilen bir halka , femurun başını tutar ve eklemde sabitler. Bu asetabulumun derinliğini arttırır.
Rahim içindeyken , bir bebeğin kalçası, femur başı asetabulumda mükemmel bir şekilde merkezlenmiş olarak gelişmelidir. Asetabulum, sanki bir bardağın içinde oturan bir topmuş gibi femur başını örtmelidir. Konjenital kalça displazisinde, asetabulumun gelişimi, özellikle bebek yürümeye başladığında, femur başının yuvadan yukarı doğru çıkmasına izin verir. Bu, sığ bir yuva ile sonuçlanır - bir fincan gibi daha az ve daha çok bir kase gibi şekillendirilir. Asetabulum femur başını yeterince örtmediği için femur yanlış yerleşimine de yol açabilir.
Bu düzeltilmezse, kalça eklemi kararsız olacaktır. Bazı durumlarda dislokasyon da meydana gelebilir. Yıllar geçtikçe, femur başı ve asetabulum doğru hizalanmadan hareket ettikçe eklemdeki kıkırdak zamanından önce ve düzensiz bir şekilde yıpranır. Sonuç, yanlış hizalamanın ciddiyetine bağlı olarak farklı derecelerde osteoartrittir. Osteoartrit, eklem başında veya soketin kendisinde oluşabilir.

Kalça displazisinin tam anatomik özellikleri kişiden kişiye değişebilir. Hem kalça soketi hem de femur etkilenebilir.
Atipik şekilli bir uyluk kemiği de kalça displazisinin bir parçası olabilir. Bu, yanlış şekillendirilmiş bir asetabulum yerine veya ona ek olarak meydana gelebilir. Femurun bilyesi ve şaftı ideal olarak birleştikleri yerde 120 ila 135 derecelik bir açı oluşturur. Ancak kalça displazisinde bu açı iki yoldan biriyle değişebilir:
- Coxa valga : Top ile femur şaftı arasındaki açı artar, genellikle 135 derecenin üzerine çıkar.
- Coxa vara : Açı 120 derecenin altına düşürülür.
Her iki durumda da uyluğun uzunluğu etkilenir - koksa vara ile kısaltılır veya koksa valga ile uzatılır. Bu, kalça ekleminde ek dengesizlik yaratır ve yürüme zorluğu, ağrı ve eklem sertliği ile sonuçlanır.
Doktorlar kalça displazisine neyin neden olduğunu tam olarak bilmiyorlar. Bununla birlikte, olası bir neden annedeki hormonal değişiklikler olabilir. Hamilelik sırasında hormonlar, doğum sırasında bebek için yer açmak ve genişlemelerine izin vermek için bir kadının eklemlerini gevşetir. Bu hormonların plasentayı geçtiği ve bebeğin bağ gevşekliğinin artmasına neden olduğu düşünülmektedir. Bebeğin anne karnındaki pozisyonu da bir rol oynayabilir - makat doğum pozisyonu ve ilk doğan çocuklarda kalçanın gelişimsel displazisi (DDH) oranlarında artış vardır. Makat pozisyonunda doğan 15 kadından birinin DDH'si vardır [kaynak: Ramsey]. Bebeğin rahimdeki pozisyonu nedeniyle sol bacak daha sık tutulur. Ebeveynleri DDH'si olan çocuklarda, ebeveynleri olmayanlara kıyasla kalça displazisi sıklığında 10 kat artış vardır [kaynak: Bjerkreim ].
Ardından, kalça displazisinin semptomlarına ve tedavisine bakacağız.
Kalça Displazisi Belirtileri ve Önlenmesi
While the term "prevention" may be controversial for a condition with congenital aspects, it's possible to diagnose dysplasia early enough in a child's life to take steps to correct the alignment. In addition, proper prenatal care to determine the position of the baby in the womb may be helpful in preparing for possible hip problems associated with breech births. Avoiding excessive and prolonged infant hip adduction, or forcing the legs in a straight position close together, may help prevent strain on the hip joints. One common source of prolonged hip adduction is the practice of swaddling.

Karl Schatz/Aurora/Getty Images
The common practice of swaddling may contribute to hip dysplasia in some babies.
The following are some of the most common symptoms of developmental dysplasia of the hip (DDH). While these are the most common, they may be experienced with differing severity. Pediatricians will screen newborns before sending them home from the hospital. In some cases, DDH is not always detectable at birth, and the baby will not present symptoms until some time later. The more common symptoms include:
- One leg may appear shorter than the other.
- The leg on the dislocated side may turn outward.
- Folds of skin on the thigh or buttocks may appear uneven.
- Distance between the legs may appear wider than normal
- There may be less mobility or flexibility on one side.
- The child may limp, toe walk or waddle.
If your baby appears to have any of these symptoms, consult your pediatrician for a diagnosis. If you or your relatives have had hip problems, an X-ray or sonogram may be appropriate, since dysplasia is more common in children of dysplastic parents.
If DDH is not detected at birth or in childhood, people will typically experience symptoms in their late twenties or early thirties. Common adult symptoms include:
- Pain in the groin region that radiates to the outer buttock or thigh
- Weakness in the leg
- Difficulty walking, possibly limping
- Loss or limitation in the joint's range of motion
- Feeling a grinding sensation in the joint
- Hearing a click or clunk sound
- Sensation of giving way, catching or locking
The process of making a diagnosis is more specific than just checking off a list of symptoms, though. Next, we'll explore how doctors diagnose hip dysplasia in children.
These are some terms you may hear in conjunction with hip dysplasia:
- DDH : developmental dislocation of the hip
- CDH: congenital dislocation of the hip
- Hip subluxation: incomplete contact between the articular surfaces of the femoral head and acetabulum
- Hip dislocation: complete loss of contact between the articular surface of the femoral head and acetabulum
- Teratologic hip dislocation: dislocation of the hip before birth
- Hip instability: the ability to subluxate or dislocate the hip with manipulation
- Displaced hip
Diagnosing Infant Hip Dysplasia
Ortolani and Barlow maneuvers have been the standard techniques for detecting hip problems in babies for the last 70 years. The Ortolani maneuver starts with the baby in a supine position -- on his or her back -- without a diaper. The physician bends the infant's hip and knees to 90 degrees. Once in this position, the doctor abducts, or moves the infant's legs apart, into the frog-leg position. If the hip is dislocated, the femoral head slides into the hip socket during this movement. There is a palpable and audible clunk as the head slips back into the socket. Each hip should be tested individually. Hearing or feeling the clunk is called a positive Ortolani maneuver.

Doctors typically screen newborns using the Barlow and Ortolani maneuvers.
In the Barlow maneuver, the physician will examine each leg individually beginning with the infant lying in the supine position. If testing the left leg, the physician will support the pelvis with the right hand. Using the left hand, the doctor will flex and adduct the left leg, or draw it across the body. The hip will gently be pushed posteriorly -- toward the back -- along the line of the femur shaft. In this case, a positive test occurs if the physician feels the femoral head slip out of the acetabulum as the hip dislocates out of the socket.
Ultrasonograms, or ultrasounds , can also be useful for diagnosis, particularly for babies under 9 months of age. Prior to 9 months, babies have little bone, and X-rays show only bone. Ultrasound also allows the doctor to see multiple angles of the joint rather than the single, two-dimensional view an X-ray provides. An ultrasound exam can accurately show the location of the ball within the socket, and the doctor can stress the hip during the examination to determine the stability of the joint. Ultrasound can also show the cartilage in infants who do not yet have a lot of bone.
Once children develop sufficient bone, X-rays tend to be used because they can more clearly show the bones of the whole hip joint in one image. This makes them more useful than ultrasound after the age of 9 months.
The process of diagnosing an adult with hip dysplasia is a little different from diagnosing an infant -- we'll look at how on the next page.
Hip Dysplasia Diagnosis in Adults
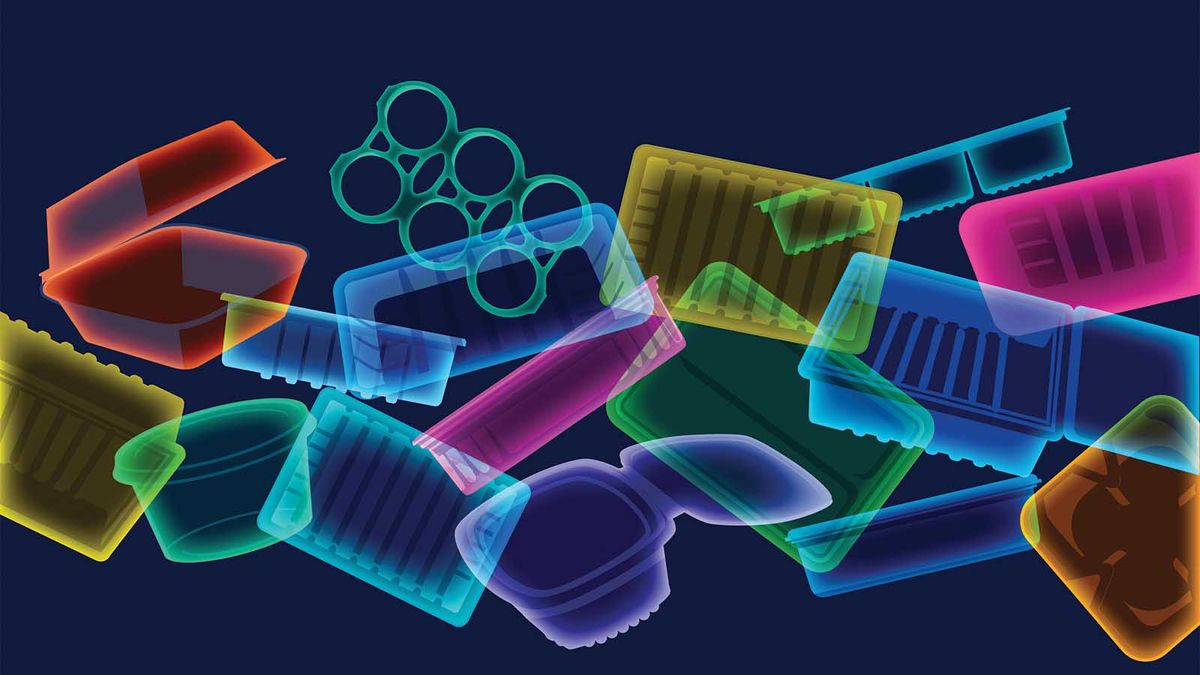
If you visit the doctor to learn if you have hip dysplasia, X-rays will be the first tool the doctor will use. An X-ray works the same way as a photo negative -- the areas containing calcium, such as bones, show up in white, and the areas containing water , such as cartilage, show up in black. The X-ray will show any abnormalities by profiling the anterior of the acetabulum. While X-rays by themselves are not accurate for hip dysplasia diagnosis, they give doctors a good method to track the progress of the hip during treatment.

Nick Veasey/Collection Mix: Subjects/Getty Images
Doctors can use X-rays of the hips to track the progress of hip dysplasia.
Like X-rays, the other tools used to diagnose hip dysplasia in adults are noninvasive and painless. One is a computer tomography scan (CT scan ). A CT scan produces multiple pictures of internal organs, soft tissue and bone with more clarity than conventional X-ray machines. These pictures can then be joined together by a computer to create cross-sectional views of the area of interest. In hip dysplasia, a CT scan, also known as a CAT scan, allows the doctor to determine how far the femur tips forward. This is called the degree of femoral anteversion. The CAT scan also lets the doctor see how well the acetabulum covers the back of the femur, known as acetabular coverage.
In a three-dimensional computer tomography scan (3-D CT scan), a computer takes the X-ray slices of the area being studied and combines them into 3-D images. These images can be rotated so a doctor can see the hip from any direction. This method is beneficial for hip dysplasia patients, since it allows the doctor to visualize the overall shape of the acetabulum for diagnosis or surgery planning.

©iStockphoto/Dean Hoch
An MRI arthrogram of the hip
Another tool is magnetic resonance imaging (MRI), which is able to visualize the underlying bone and soft tissue anatomy in any plane or angle with greater contrast than a CT scan. An MRI arthrogram adds a contrast or radiology dye to the MRI process in order to acquire better images of a joint. An MRI arthrogram is done in two parts. First, the patient lies on an X-ray fluoroscopy table, which provides real-time X-ray images to guide the radiologist as he or she injects contrast solution into the joint. The doctor can also move the hip around during the arthrogram to help detect tears to the labrum and assess the mobility of the hip and its reducibility, or potential to be corrected. However, this is not always done during an arthrogram -- it depends on what your surgeon has ordered to be tested. This stage roughly takes 30 minutes to complete. The patient is then taken to the MRI scanner for the rest of the procedure.
Once the doctor has evaluated all the medical images, he or she can make a diagnosis. The recommended course of treatment varies considerably based on whether the patient is a baby or an adult, among other factors. On the next two pages, we'll explore how doctors treat hip dysplasia noninvasively, beginning with treatment in children.
Many people who have been diagnosed with hip dysplasia have shared their experiences with other patients through blogging. Here's a sample:
- I am PAO'd
- Paper or Dysplastic?
- My So-called Dysplastic Life
- Periasetabular Osteotomi Dergisi
- Topallanmak ya da Topallanmamak
- PAO Hikayem
- trajik bir şekilde kalça
- Avustralya PAO Dergisi
- Hip-hop Anonim
Çocuklarda Ameliyatsız Kalça Displazisi Tedavisi
Çocuklarda kalça eklemlerini düzeltmek için çeşitli yöntemler mevcuttur. Çocuğun yaşı ve semptomların şiddeti en iyi tedavi yöntemini belirleyecektir. Doğumda displazi tespit edilirse prognoz olumludur ve çeşitli cerrahi olmayan seçenekler vardır. Daha sonra tartışacağımız cerrahi müdahaleler de vardır.

Pavlik emniyet kemeri, kalça displazisi olan bebekler için standart bir tedavidir. Kalçaları doğru bir şekilde geliştirmelerini sağlayan bir pozisyonda tutar.
Pavlik emniyet kemeri 6 aya kadar olan bebeklerde kullanılır. Bir göğüs kemeri, iki omuz askısı ve kanvas, Velcro ve tokalardan yapılmış iki üzengi. Emniyet kemeri, uyluğu yuvaya doğru açıda yerleştirir ve bacakları ayrı tutar. Bir doktor, doğru şekilde oturması için emniyet kemerini takacak ve muhtemelen bebeğin 6 ila 12 hafta boyunca günde 24 saat takmasını önerecektir. Kalça çıkığı olan bebeklerde, emniyet kemeri daha kısa süre giyilebilir. 6 aylıktan küçük bebeklerde Pavlik emniyet kemerinin başarı oranı yüzde 85 ila 95'tir.
Çekiş , çocuğun bacaklarını çeken iplere bağlı ağırlıkları kullanır. Bu, bir zamanlar kalça displazisi için yaygın bir tedaviydi, ancak bugün tipik olarak yalnızca Pavlik koşum takımı başarısız olduğunda veya kalça displazisi 6 aylıktan sonra teşhis edildiğinde kullanılmaktadır. Femur çıkıksa, çıkığın etrafındaki kaslar gerilir ve femurun yuvaya geri dönmesi imkansız hale gelir. Çekiş, doktorun uyluğu yeniden hizalayabilmesi için kasları zamanla nazikçe gerer. Çekiş olmadan kaslar, vücut alçısında bile femuru yuvadan dışarı çekebilir. Çekişin uzunluğu, kısa molalarla günde 24 saat, birkaç günden birkaç haftaya kadar değişir. Bu süreç rahatsız edici ama acı verici değil.
Bu yöntemler başarılı olmazsa veya çocuk büyür ve çıkık tekrarlarsa, doktorun uyluğu sokete manuel olarak yerleştirmesi gerekebilir. Buna kapalı redüksiyon denir . Bu işlem kalçanın kesilmesini gerektirmez. Bununla birlikte, bazı durumlarda tenotomi gerekir - cerrah kalçanın hareketliliğini artırmaya yardımcı olmak için bir kesi yapar ve gergin tendonları keser. Kalça daha sonra femur başını asetabuluma geri getirmek için harici olarak manipüle edilir. Kalçayı stabilize etmek için bir spika alçı uygulanır.
Spica alçı eklemi hareketsizleştirir ve kemiklerin ve tendonların iyileşmesini sağlar. Döküm alçı veya fiberglastan yapılmıştır ve genellikle rahatlık için pamuklu bir astara sahiptir. Bazı durumlarda, bir cerrah cildi kuru tutmaya çalışmak için Gore-Tex'i kullanabilir. Birkaç çeşit başak dökümü vardır. Tipik olarak göğüsten başlarlar ve bir veya iki kalçayı kaplarlar veya bir tarafta bacaktan aşağı inip diğer tarafta kalça veya dizde durabilirler. Cerrah, kullanılacak en iyi alçıyı belirleyecektir. Spica alçı 4 aya kadar giyilir, ancak bir doktor genellikle büyümeye izin vermek ve hijyene yardımcı olmak için 6 haftada bir değiştirir.
Bazı doktorlar da farklı zamanlarda veya farklı sıralarda diş teli veya atel kullanacaktır. Nihayetinde, doktorun talimatlarını ve belirli diş tellerini kullanmanın gerekçesini anlamak ebeveyne kalmıştır. Braketler ve ateller, malzemelerine ve bakım ve kullanım talimatlarına göre farklılık gösterecektir. Bir destek, bir Pavlik koşum takımının bir sonraki adımı olabilir ve bazen bir başparmak kalıbı çıkarıldıktan sonra da kullanılır. Bazı durumlarda, bir çocuğun alçı çıkarıldıktan sonra bir korse ihtiyacı yoktur. Cerrah buna küçültme ve alçının sonucuna göre karar verecektir. Tüm bu braketlerin genel adı abduksiyon ortezidir .
Kalça displazisi gelişimsel bir kemik bozukluğu olduğu için tedavi edilmezse zamanla bozulmaya devam edecektir. Displazinin ne zaman teşhis edildiğine bakılmaksızın, yaşam boyunca düzenli olarak gözden geçirilmesi ve yeniden değerlendirilmesi gerekecektir. Ardından, yetişkinler için mevcut olan cerrahi olmayan tedavilere bakacağız.
Erişkinlerde Ameliyatsız Kalça Displazisi Tedavisi
Kalça displazisi olan yetişkinler için birçok cerrahi olmayan tedavi, iltihabı azaltmaya veya eklem sağlığını desteklemeye odaklanır. Genellikle tek bir besin takviyesi olarak satılan glukozamin ve kondroitin sülfat eklem sağlığı için alınabilir. Oral glukozamin, kabuklu deniz hayvanlarından elde edilir (vejetaryen seçenekler olsa da) ve kıkırdağın yeniden inşasına yardımcı olabilir. Kondroitin sülfat ayrıca kıkırdağın önemli bir bileşenidir. Her ikisi de eklem ağrısını azaltabilirken , osteoartrit tedavisinde etkinlikleri hakkında çelişkili raporlar vardır.

© iStockphoto /Sebastian Kaulitzki
Kalça displazisi için pek çok girişimsel olmayan tedavi, rahatsızlığı ve ağrıyı azaltmayı amaçlar.
Diğer bir alternatif tedavi, iltihabı azaltabilecek bir anti-inflamatuar diyettir . Zencefil , sarımsak , zerdeçal ve yeşil çay diyete eklenebilir veya takviye olarak alınabilir. Omega-3 yağ asitlerinin iltihap önleyici etkileri olabilir ve balık ve balık yağı takviyelerinin yanı sıra keten tohumu , kabak, karalahana, fındık , brokoli , karnabahar ve ıspanakta bulunabilir. Öte yandan, itüzümü ailesindeki bazı yiyecekler eklem sorunları olan kişilerde iltihaplanmayı artırabilir. En yaygın yenen itüzümü domates , patates , patlıcandır .ve kırmızı biber. Tomatillos , tamarios, pepinos, yenibahar, kırmızı biber, kırmızı biber ve Tabasco sosu da itüzümü alkaloidleri içerir. Ulusal Ücretsiz ve Alternatif Tıp Merkezi tarafından desteklenen anti-inflamatuar diyetin etkinliğini belirlemek için bir çalışma şu anda devam etmektedir [kaynak: NIH ].
Reçetesiz satılan iltihap önleyici ilaçlar , NSAID'lerin (steroidal olmayan iltihap önleyici ilaçlar) genel başlığına girer. NSAID'lerin uzun süreli, büyük kullanımı gastrointestinal tahrişe veya daha ciddi bağırsak ve böbrek rahatsızlıklarına yol açabilir . Ağrı kesici ilaçlar semptomların şiddetini azaltmaya yardımcı olsa da kalçadaki bozulmayı durdurmaz.
A doctor can also give steroid shots to reduce inflammation. The decrease in inflammation reduces the level of pain. The most common side effect is a condition called cortisone flare -- the injected cortisone crystallizes and becomes painful for a day or two. Some studies have shown that repeated use of cortisone can weaken tendons and soften cartilage, so a doctor may limit the number of injections. Many doctors consider cortisone injections to be a temporary solution on the path to surgery and may not recommend them.
There are also simple, physical steps a person can take to relive the pain associated with hip dysplasia:
- Ice numbs the area and can help reduce inflammation. Do not leave ice on any location for longer than fifteen minutes.
- Regular, low- or non-impact exercise such as swimming, aquatic therapy or cycling can encourage strength and range of motion. Strong muscles will act like shock absorbers and provide greater support for the hip. If you're starting an exercise program, be sure to discuss it with your doctor or physical therapist.
- Yoga strengthens and stretches muscles and improves overall muscular health. The psychological benefits can also improve a person's well-being when coming to terms with the disability of hip dysplasia, which often presents itself at a relatively young age. However, it's important to choose a method that focuses on slow movement and optimal physical alignment, such as the Anusara or Iyengar methods. Hatha, gentle or basics classes are generally good for beginners. Avoid Vinyasa, Power Yoga and Hot Yoga, (unless you're experienced and able to modify poses to support the hip), as these classes will emphasize a faster pace with less focus on individual alignment.
- The hip joint deals with three times the amount of force relative to body weight. For example, in someone weighing 150 pounds (68 kilograms), the hip will deal with 450 pounds (204 kilograms) of force. Weight loss for those who are overweight can significantly reduce the stress on the hip joint, since a 5-pound (2.3-kilogram) loss would result in 15 pounds (6.8 kilograms) less force on the joint [source: Klapper and Huey]. Any weight loss program undertaken to support the hip should be with the supervision of a doctor or specialist.
- Physical therapy, massage and bodywork can all help to increase muscular strength and flexibility in and around the joint and reduce joint pain. Regular physical therapy can strengthen individual muscles and teach the body how to better align itself, while massage and bodywork can increase range of motion and reduce pain by releasing muscles in spasm.
In adults, nonsurgical intervention can be useful for pain management when the joint hasn't deteriorated to a point that surgery is necessary. However, it's important not to prolong the waiting time beyond the point when the cartilage can support surgical procedures. Now, we'll take a look at those procedures.
Hip Dysplasia Surgery
As symptoms of hip dysplasia worsen, a doctor and patient may consider two categories of surgeries. The first reshapes, redirects or salvages bone in order to preserve the natural joint for as long as possible. The second, total hip replacement (THR), replaces the entire joint and is used in cases of severe pain, considerably compromised mobility and cartilage that is so worn that replacement is necessary. Many surgical procedures can prolong the amount of time before the patient needs a THR. This has several advantages:
- Using their own bone and cartilage allows for a live joint with full sensation.
- There are no activity restrictions.
- Bone is preserved rather than lost to an artificial joint.
- A proper "roof" is created so that if a THR is needed later on it should be successful.
- There is no worry about the possible effects of metal decomposition of an artificial joint for either the patient's body or a fetus, as this surgery is often performed on women of childbearing age.
Children have two surgical options: soft tissue surgery and bone surgeries, also known as osteotomies. One soft tissue surgery is open reduction. This is the surgical option for children over the age of 2 at the time of their first diagnosis, or for those whose closed reduction failed to correct the joint. In an open reduction, the surgeon cuts into the hip capsule and re-positions the femoral head. Once the hip is sutured, a spica cast is applied for 4 months or longer to stabilize the hip. Open reductions and other soft tissue surgeries like tendon lengthening are normally only an option in babies and very young children.
Once children are a little older, there are bone surgeries, including reshaping and redirecting:
- Reshaping reshapes the actual hip socket and is performed on young patients whose hips are pliable. These osteotomies include Dega, Pemberton, San Diego and acetabuloplasties.
- Redirecting is performed on older patients who no longer have pliable bone. In these cases, the surgeon repositions the socket but does not change its shape. These osteotomies include the periacetabular, spherical, triple and others.
There are also salvage procedures, like a shelf and Chiari osteotomy, in which non-articular cartilage is used to help hold the hip in place. The cartilage added in these procedures is fibrocartilage rather than true articular cartilage. In severe cases of dysplasia, avascular necrosis (AVN), in which poor blood supply leads to bone death or arthritis , can occur. In such cases, or in cases where the hip socket is misshapen or small, a shelf and Chiari osteotomy may be the only alternative. Another salvage option is an arthrodesis, or fusion, which eliminates all motion of the hip. This procedure is used mostly in young, active patients with poor cartilage.
Osteotomies can realign the weight-bearing surfaces of the joint while maintaining the natural bone. They can be performed on the pelvic bone or the thigh bone, or both. A surgery on the femoral side of the joint is a femoral osteotomy. One on the acetabulum side is a pelvic or innominate osteotomy. On the following pages, we'll look at two ostotomies that use these two approaches.
Arthroscopy is a surgical procedure often performed on the soft tissue surrounding the joint. It's a minimally invasive procedure that can postpone more invasive surgery. In some cases where the dysplasia is relatively non-advanced, arthroscopy can rule out the need for further surgery altogether. Arthroscopic surgery is a relatively short procedure, and often the patient will go home the same day.
For a patient requiring either an osteotomy or replacement/resurfacing, arthroscopy can address painful soft tissue conditions and greatly improve the health of the hip. Such conditions include:
- Loose bodies: In a joint with arthritis, the formerly smooth surface of the cartilage cracks, and pieces of cartilage can break off and float in the joint. These loose bodies cause the joint to catch. They also scratch the still-smooth cartilage.
- Torn labrum: The thick rim of cartilage around the socket can tear and partially flip itself into the joint, scratching the cartilage. Arthroscopy can trim the labral tear and stop it from damaging the cartilage.
- Synovitis: The synovial membrane, a lubricating layer of tissue, can become inflamed and cause disabling pain, requiring removal. Arthroscopy can be used to remove portions of the synovium. However, a complete synovectomy (removal of entire synovium) is not possible with arthroscopy.
Bernese Osteotomy or Ganz Procedure or Periacetabular Osteotomy (PAO)
There are a variety of pelvic osteotomies used to treat hip dysplasia. Some are used only on children, while others treat specific bone structure and reconstruction needs. Already popular in Europe, the Bernese, also known as the Ganz procedure or periacetabular osteotomy (PAO), has become a common treatment for adults in the United States. It was first performed in 1984 in Bern, Switzerland by doctors Reinhold Ganz and Jeffrey Mast. This operation can be performed on children over the age of 10 as well as on adults, usually under age 40.

Photo courtesy Lauren Giovannoni and Sarah Court
This X-ray shows a hip after PAO surgery.
Bernese PAO is used in situations where the roof of the acetabulum does not cover the head of the femur the way it should. Using a series of controlled cuts, the surgeon separates the acetabulum from the pelvis. That's where the procedure gets its name -- "periacetabular" simply means "around the acetabulum." The surgeon can then rotate the acetabulum into a better position to cover the femoral head. During surgery, the doctor can also make subtle changes, such as increasing the amount of coverage in the front of the joint, or the anterior coverage. This surgery generally takes 4 to 5 hours depending on whether additional procedures are performed at the same time. Research suggests that a PAO can halt the destruction of the joint or prolong the use of the joint for those in early adulthood, postponing the need for a total hip replacement (THR).
After surgery, the patient will use crutches with minimal weight bearing on the affected leg for the first 6 to 8 weeks, followed by weight bearing with a crutch or cane until it's no longer needed. Physical therapy and the strengthening of the leg will take several months since muscles and tendons are affected by the surgery and weaken with lack of use.
The Bernese PAO also has advantages over other surgical options:
- It allows for a large correction in the coverage and containment of the femoral head.
- It's performed through one incision.
- It does not dramatically change the shape of the pelvis.
- It allows for future vaginal childbirth .
- It keeps the posterior column of the pelvis intact, allowing the patient to walk soon after the surgery and ensuring that the blood supply to the acetabulum remains uninterrupted.
- The surgeon can examine the acetabular labrum and repair it, if needed, through the same incision.
As with any surgery, there is a small risk of complications. The bone may not rejoin along the break, or abnormal bone may form on non-bone tissues. This abnormal bone is known as heterotrophic bone and can severely affect the joint's range of motion. This complication requires additional surgery. There are also several conditions that can arise as complications:
- Femoral nerve palsy is the loss of movement or sensation in the leg caused by damage to the femoral nerve .
- Intra-articular fracture is a break that crosses into the joint surface, resulting in a varying amount of cartilage damage.
- Deep vein thrombosis is caused by a blood clot that usually starts in the leg, breaks off and causes a pulmonary embolism in the lung . Blood thinning medication, tension stockings and movement soon after surgery all help to reduce this risk.
Femoral Osteotomy (FO)
A femoral osteotomy (FO) is any surgical procedure that cuts through the femur to change its relationship to the hip or to the knee. To treat hip dysplasia, the doctor cuts through the femoral head and rotates it anteriorly or posteriorly -- to the front or to the back. This creates better coverage of the acetabulum over the femoral head. An L-shaped plate and several pins reattach the femoral head to the femoral body. The bone knits back together with this support in place.

Photo courtesy Lauren Giovannoni and Sarah Court
This X-ray shows a hip after FO surgery.
Due to the plate and pins, an external body cast is not necessary. The patient will spend several weeks post-surgery using crutches and several months in physical therapy to strengthen the hip and leg muscles. Follow-up X-rays will determine the progress of the femoral head as it knits itself to the femoral body. After a year, an optional second surgery can be performed to remove the metal plate. This surgery can be performed in conjunction with a periacetabular osteotomy (PAO) if needed to create the best possible femoral-acetabular coverage. Labrum repair and other soft-tissue arthroscopic procedures may also be performed at the time of surgery.
The FO was developed in the early part of the 20th century, so it isn't performed as often as the more recently developed PAO. However, for patients whose dysplasia has as much to do with the angle of the femoral head (coxa vara or coxa valga) as with the shape of the acetabulum, it can be the appropriate choice. As with any osteotomy, there are short- and long-term benefits to using the patient's own bone.
The surgery is a 2- to 3-hour procedure. An incision is made on the outside of the hip, and the vastus lateralis muscle, which is part of the quadriceps, is lifted to access the femur beneath. This is typically the only muscle affected by the surgery, which reduces the severity of nerve damage in the area.
Once postoperative swelling has diminished, the patient will be aware of the plate to a varying degree, depending on individual sensitivity and physical size. Awareness and daily discomfort are the major factors that contribute to the decision to undergo a second surgery to remove the hardware. In any event, the plate must stay in place for 12 months to give the bone sufficient opportunity to heal.
The second surgery is relatively simple: The surgeon goes in about halfway along the initial incision and removes the plate and pins. The largest hole created by the top of the metal pin in the femoral head is filled with synthetic bone filler, and the lower holes fill in on their own, requiring another, shorter period of time on crutches post-surgery. Overall, however, this surgery requires far less hospital time and physical therapy than other surgeries.
Major complications include infection, neurovascular injury, nonunion of bone, inability to obtain or maintain a full correction, postoperative pain and continued degeneration of cartilage. Other complications include deep vein thrombosis and painful hardware. However, the likelihood of any of these complications is roughly 1 percent.
Overall, hip range of motion, gait, pain, leg-length discrepancy and patient satisfaction are improved from femoral osteotomy, and a successful surgery may reduce or even entirely remove the need for a total hip replacement (THR) during the patient's lifetime. However, should a THR become necessary, the FO, like the PAO, supports the necessary alignment of the hip joint. Next, we'll examine the use of THR as a treatment for hip dysplasia.
Hip Replacement for Hip Dysplasia
Typically, hip replacement surgeries are considered when pain from osteoarthritis, caused by the normal aging process , drastically affects quality of life. Hip dysplasia can speed up this wear on the cartilage, making a total hip replacement (THR) necessary. A condition called avascular necrosis (AVN), caused by a loss of blood supply to the femoral head, often also necessitates a hip replacement because of the death of cartilage.

Patients with hip dysplasia may undergo hip replacement to completely replace the affected hip with a prosthesis.
The materials used to make artificial hip joints have changed significantly since the 1920s. Originally, an artificial socket was made from plastic , and a femoral head and neck were made from cobalt-chrome. Today, titanium has become more common than cobalt-chrome. Regardless of the metal type, the plastic socket wears away at roughly 1 millimeter per year against the metal ball, thus limiting the life of the artificial hip to 10 to 15 years. New plastics are thought to wear out a lot slower, but at this point there is no long-term data to prove if they last longer. Newer developments include metal-on-metal joints and ceramic-on-ceramic joints.
The basic design of the prosthesis is similar regardless of the materials or the manufacturer, and the surgery itself is unchanged by the materials used. The surgeon removes the femoral head and neck through an incision over the hip joint. He or she then inserts an angled shaft with a smooth, balled implant into the bone. The next step is to smooth out the socket side of the joint and fit it with a cup. Depending on the type of artificial joint being used, the cup will either be cemented into place with bone cement or left uncemented. The cementless joint is made in such a way that the bone naturally grows into the surface to keep it in place.
For those with hip dysplasia, there needs to be roughly 70 percent contact of the cup to the socket bone. In some cases, hip dysplasia patients do not have enough of a "roof" in the hip for this surgery to be successful.
There are several possible complications of hip replacement:
- Dislocation is most likely to happen in the first 6 weeks after the surgery. However, as an artificial joint lacks the depth of the natural joint, it will always be easier to dislocate an artificial joint than a natural one. Your surgeon will give you a list of short-term and long-term precautions and range of motion limitations to help avoid dislocation.
- Infection is a rare but serious occurrence. Antibiotics are usually given before and after surgery to lessen this risk.
- As with the surgeries discussed previously, deep-vein thrombosis is a potential complication.
- Loosening of the joint over time is likely to result in the need for a revision surgery. The activity level of the patient and artificial hip materials used will help to determine the overall life of the joint.
Over the last 5 years, minimally invasive total hip replacement (THR) been used in hip replacements. Instead of a 6- to 8-inch (15- to 20-centimeter) incision, it uses two smaller incisions to attach a standard, cementless replacement. There are some advantages to minimally invasive THR:
- A shorter hospital stay with a faster rehabilitation (outpatient surgery has been achieved in both the U.S. and U.K.)
- Decrease in pain due to less muscle, tendon and ligament trauma
- Improved cosmetic appearance due to shorter scars
- Ability to use standard implants that have an established track record
Read on to learn about what happens when THRs start to wear out.
Hip Replacement Revision and Hip Resurfacing
Unfortunately, the majority of THRs have a limited life. The success of a revision later on relies on the quality and quantity of available bone. Regular check-ups and X-rays to make sure the hip is working well will keep the revision relatively simple. Most, however, are caught when a fracture or dislocation occurs, making the revision more complex. In cases where there is not enough viable bone, grafts or special components are needed.

Charles McRae, M.D./ Visuals Unlimited/Getty Images
Hip replacement revision is often required after normal wear and tear. Issues like fractures and dislocations (shown) make revision more complicated.
Revision surgery comes with a few disadvantages:
- The original component needs to be removed and new components put in its place, making for a longer surgery.
- Longer incisions are often needed.
- There is greater blood loss and post-operative pain.
- Older patients' health and strength may compound problems.
Long-term results are typically excellent. However, complications are a little more frequent than with the original surgery. For patients who are young when they undergo a hip replacement, revision surgery is almost inevitable. However, the newer materials available seem to improve the overall life span of the artificial joint, lessening the number of necessary revisions.
Hip resurfacing is a newer hip replacement procedure with advantages for younger patients. Due to their age, these patients may need more than one procedure in their lifetime. Rather than removing the head and neck of the femur, only the head is trimmed, and a round metal cap is placed on it. The socket is fitted with a metal cup, and the body's own natural fluids lubricate the artificial joint.
The advantage of this procedure is that far less bone is removed, allowing for less complex and more successful future revisions. In a younger, more active patient, hip resurfacing uses a larger metal head, which helps to lower the risk of dislocation.
This procedure is relatively new. The first surgery of its kind was performed in Europe in 1997 and was only FDA approved in the U.S. in 2006. This means there is no long-term data regarding the surgery's success rate, although medium-term data looks promising. There is also a 2 percent risk of the femoral neck fracturing in the first 6 months. Hip resurfacing is not suitable for people with or at risk of osteoporosis . Hip resurfacing requires more than 70 percent contact between the bone and metal socket, and thus is not always an option for people with hip dysplasia.
Procedures like femoral osteotomy and periacetabular osteotomy can take care of hip dysplasia symptoms, like pain and range of motion difficulties, and they can prolong the amount of time before a necessary THR. But they do not actually fix the structural problem of a shallow socket. In these cases, the surgeon may determine that resurfacing is not a viable option only once the patient is on the table. In such cases, the doctor may choose to perform a replacement instead to avoid future dislocations and instability of the joint.
To learn more about hip dysplasia, follow the links on the next page.
Lots More Information
Related Articles
- How Muscles Work
- How Exercise Works
- How FOP Works
- How Osteogenesis Imperfecta Works
- How X-rays Work
- How MRIs Work
- How CAT Scans Work
- How do broken bones heal?
More Great Links
- Hip-baby.org
- Hip Universe
- Kalça ve Pelvis: Hasta Eğitimi
- orthoseek
Kaynaklar
- Amerikan Ortopedi Cerrahları Akademisi. "Kalça Osteoartriti." 7/2007.
http://orthoinfo.aaos.org/fact/thr_report.cfm?thread_id=208&topcategory=Artrit - Amerikan Ortopedi Cerrahları Akademisi. "NSAID'ler nelerdir?" 10/2004.
http://orthoinfo.aaos.org/fact/thr_report.cfm?Thread_ID=398&topcategory - Bjerkreim I. Norveç'te kalça ekleminin konjenital çıkığı. Acta Orthop Scand 1974;Ek 157.
- Sedirler-Sina. "Kalça Artroskopisi."
http://www.cshs.org/460.html - Duke Ortopedi. "Pavlik Koşum Takımı."
http://www.wheelessonline.com/ortho/pavlik_harness - Duke Ortopedi. "Wheeless' Ortopedi Ders Kitabı." Osteotomi.
http://www.wheelessonline.com/ortho/search?search=osteotomy&go.x=0&go.y=0 - Dunn, Harold K. MD. "Kalça Erken Artrit için Pelvik Osteotomi." Medscape Bugün.
http://www.medscape.com/viewarticle/421043 - Fragomen, Austin T. "Femoral Osteotomi." eTıp. 7/13/2006.
http://www.medicine.com/orthoped/topic85.htm - Hart, Erin ve ark. "Kalça Gelişimsel Displazisi (DDH)." Massachusetts Genel Hastanesi.
http://www.massgeneral.org/ORTHO/Hip_Dysplasia.htm - Önce Sağlık. "Spika Dökümü." 6/2000.
http://www.health-first.org/health_info/your_health_first/kids/spica_cast.cfm - HipHelp.
http://www.hiphelp.com - Huddleston, Dr. HD "Kalça Eklemi Artriti."
http://www.hipsandknees.com/hip/hipimplants.htm - Klapper, Robert MD ve Lynda Huey. "Kalçalarını İyileştir" Wiley. 1999.
- Diz Sözlüğü.
http://www.kneeguru.co.uk/dictionary/doku.php/f/femoral-osteotomi - Larson, Jeffrey P. ve ark. "Konjenital Kalça Displazisi." Sağlık hattı. 2006.
http://www.healthline.com/galecontent/congenital-hip-dysplasia - Laude, Frederic. "Periasetabular Osteotomi."
http://www.hanchegenou.com/us/orthop_hanche/periacetabulaire/periacetabulaire.php - Laurence, Jeremy. "Yeni CT Taraması Gövde İçine 3D Bakmaya İzin Veriyor." Bağımsız. 26.11.2007.
http://news.in Independence.co.uk/health/article3196259.ece - McCarthy, James J. "Kalça Gelişimsel Displazisi." eTıp. 6/3/2008.
http://www.medicine.com/orthoped/topic456.htm - Orthoseek. "Kalça Displazisi."
http://www.orthoseek.com/articles/hipdys.html - Pediatrik Ortopedi. "İnnominate Osteotomi."
http://www.pediatric-orthopedics.com/Treatments/Hips/Innominate/innominate.html - Radyoloji Bilgisi. "Bilgisayarlı Tomografi - Vücut." 27.03.2007. http://www.radiologyinfo.org/en/info.cfm?pg=bodyct
- Ramsey PL, Lasser S, MacEwen GD. Kalçanın konjenital çıkığı. Yaşamın ilk altı ayında çocukta Pavlik emniyet kemeri kullanımı. J Kemik Eklem Cerrahisi Am . Ekim 1976;58(7):1000-4
- Tan, E. "Omega-3 Yağ Asitleri." Huntington'un Stanford'da Eğitim için Sosyal Yardım Projesi.
http://www.stanford.edu/group/hopes/treatmts/antinflm/i5.html - Artrit Derneği. "Femoral Osteotomi." 20/12/2007
http://www.arthritis.ca/tips%20for%20living/exploring%20surgery/exs13/femor/
default.asp?s=1 - Kaliforniya Üniversitesi, San Francisco. "Pediatri: Kalça Displazisi."
http://orthosurg.ucsf.edu/public_site/sindex.cfm?page_ID=pediatrics&article_ID=51 - University of Iowa Department of Orthopedics. "Total Hip Replacement: A Guide for Patients." December 1999.
http://lib.cpums.edu.cn/jiepou/tupu/atlas/www.vh.org/adult/patient/orthopaedics/
hipreplace/index.html - University of Washington Medical Center. "MRI Arthrogram."
http://www.uwmedicine.org/PatientCare/MedicalSpecialties/SpecialtyCare/
UWMEDICALCENTER/Radiology/mriarthrogram.htm - Wellington Hospital Hip Unit. "Surgery at the Wellington."
http://www.thewellingtonhipunit.com/surgery.asp - Zimmer. "X-rays." 3/29/2006.
http://www.zimmer.com/z/ctl/op/global/action/1/id/8016/template/PC/navid/166